What’s your Fertility Plan and do you qualify for IUI?
Welcome to this free 6-part article series designed to help you determine your fertility plan and understand the steps you can take to optimise your fertility outcomes. Below you’ll find Part 5 – “What is IUI & do you Qualify?” If you’ve already read articles 1 to 4, feel welcome to skip this intro and get stuck into part 5 below. If this is, however, your first time finding out about this series – please read on to learn what it’s about, how it can help you and what to expect over the coming weeks.
Over this free 6 week article series we are going to discuss all potential options for those of you who are:
In these articles I will address information around:
Opportunity to Ask Me Questions – LIVE
After each article release, you have the option to submit any questions you may have by 7pm Monday evening to the Create A Fertile Life Facebook group. If you’ve not yet joined that private group you are welcome to go there and request to join.
If you wish to submit your questions anonymously, you can private message the Fertile Ground Health Group Facebook page and admin will forward them to me.
Each Tuesday, I will be answering your questions live in this Create a Fertile Life Facebook group at 7pm AEDT, so we can all learn from each other.
Now, some of you may know exactly what your plan is, others may not have thought about it so concisely yet. Whatever stage you are at, I want you to provide you with the tools to determine what your fertility plan can look like and how you can optimise your outcomes with Naturopathy. Grab a pen and a piece of paper, or type in to a document on your phone/computer so that you can create the skeleton of the items that relate to YOUR individual journey and we will build on this each week over the 6 weeks of this series.
I am excited to be on this journey with you. If you’ve already registered for the whole free package, take a sneak peek at part four below and check your inbox for the arrival of your full comprehensive article for this week (week 5).
If you’re just finding this free series now and would like access from part 1 all the way to part 6 – simply register here for your free access to the whole package.
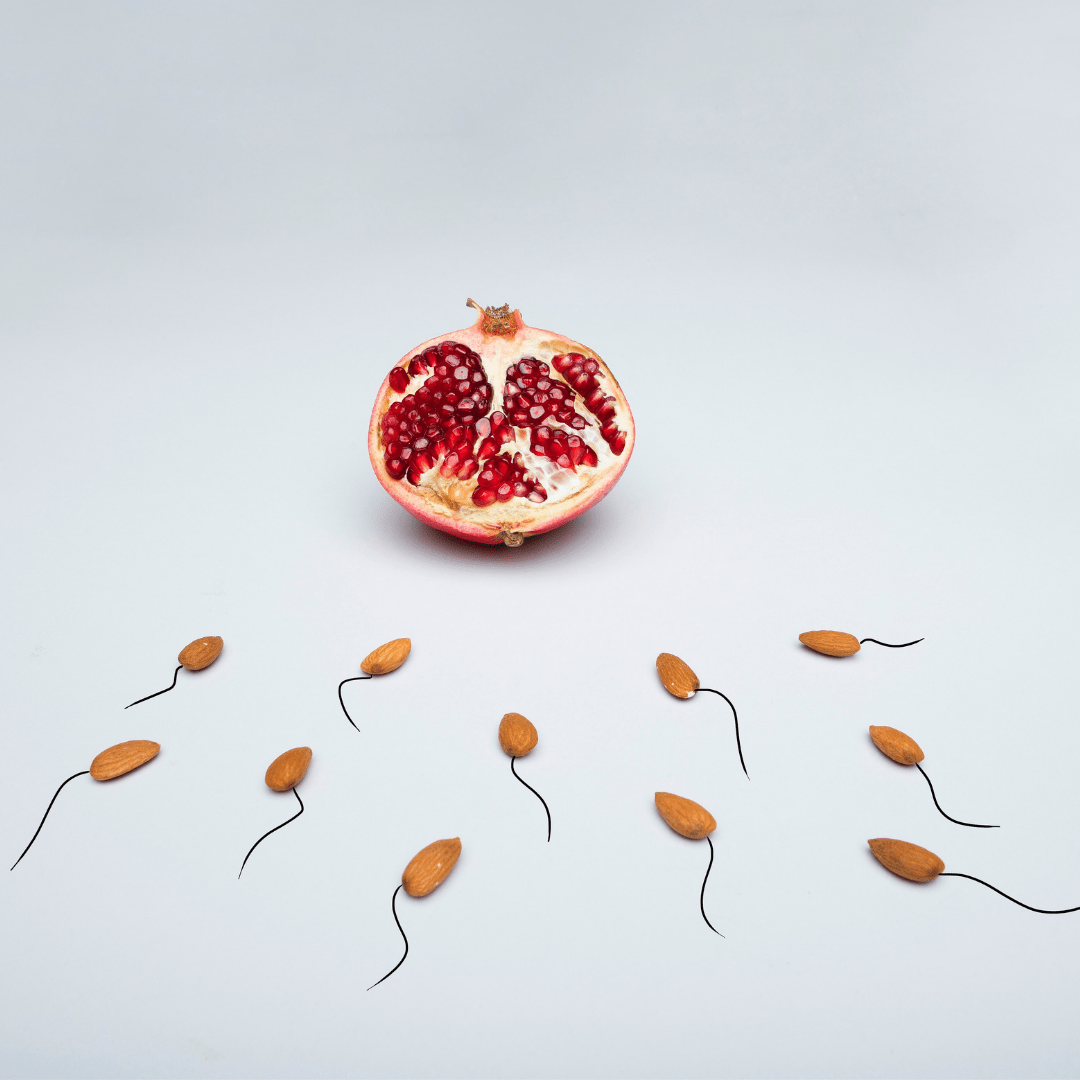
IUI is also known as Assisted or Artificial Insemination (AI), as it is the process of assisting sperm to inseminate into the uterus at ovulation. The two key aspects of IUI include washing the sperm to find the best quality sperm, and timing the insemination procedure to coincide with when you’re ovulating. (2)
Firstly, the sperm sample (from either a partner or known/clinic recruited sperm donor) is washed to find the most active and virile sperm. It is then inserted through the cervix and into the cavity of the uterus via a catheter at ovulation. You could say that the IUI process gives the sperm an advantage in quality, combined with a head start by selecting the highest quality sperm from the sample provided; with insemination increasing the number of sperm that reaches the fallopian tubes. While the sperm still need to find their way to the egg on their own for fertilisation, the greater the quality and number of sperm that reach the tubes, the greater chance of fertilisation occurring. (1,2)
Secondly, your cycle is monitored to determine if/when ovulation is occurring. To refresh your memory, ovulation occurs when an egg is released from one of your ovaries and must occur in order for conception to be successful. In the same way that timing intercourse during your fertile window is important for couples whom can provide both the egg and sperm, IUI is conducted at the time of ovulation by closely monitoring ovulation using blood tests and ultrasound to track the developing follicle to determine when insemination will go ahead.
Sounds easy, right? Reproduction always seems so straight forward on paper. But unfortunately for some, and particularly in a world where sperm quality is on the decline due to today’s way of living and environmental factors, it’s a lot more complex. So if IUI assists to find the best quality sperm prior to insemination, what if the quality of sperm is poor to begin with?
If the quality of the sperm sample is poor, then it’s like selecting the ‘best of a bad bunch’ so to speak. Now that it’s week five and I’ve spent all this time going on about the importance of preconception care, please bear with me while I repeat myself… this is why preconception care is so important! We want to be able to holistically assess all the contributing factors to sperm quality to be able to control and optimise those variables as much as possible. We want to have the best quality sperm sample to select from in the first place. We want the best of the best! But more on this and egg quality later…
The IUI process is described as similar to a pap smear in sensation. A speculum is inserted into the vagina so the cervix can be visualised. A thin catheter containing the selected sperm is then passed through the cervix and into the uterus. The process takes a few minutes to complete, usually with minimal discomfort. IUI does not require sedation. (3,4)
For single cis-women, or individuals or couples assigned female at birth who require donor sperm, IUI is the ART method that is most commonly used. IUI may also be indicated in cases of mild suboptimal semen volume, sperm count, and/or sperm motility, mild Endometriosis, cervical scarring or other concerns that may reduce sperm penetration into the uterine cavity, poor or absent cervical mucous, for those who cannot have regular or penetrative sex, infertility of unknown cause, and for individuals for which ovulation is absent or irregular. (3)
IUI is not indicated for significant sperm quality issues where a good sperm sample cannot be achieved in the andrology laboratory, or for individuals with poor fallopian tube functioning or blockages – these need to be open and functioning for the sperm to be able to reach the egg. (4)
In mild cases of poor sperm quality, while IUI washes and selects the most viable sperm and gives sperm a bit of a helping hand in helping them get closer to where they need to go, it in no way improves sperm quality parameters on a cellular level. This is why focusing on improving all parameters of sperm quality where possible is such an important preconception consideration prior to undertaking IUI.
For those of you using your partner’s or known donor sperm, I hope this gives you some encouragement to at least have a conversation with them about undertaking a semen analysis prior to giving their sample for IUI. Hopefully your partner is open to undertaking preconception care alongside you, and your donor may or may not be open to it. But it’s absolutely worth a discussion to optimise your outcomes and require less samples from them! Even better if your donor is open to 3 months (only 12 weeks) of preconception care to improve their sperm quality. If they need a little convincing, I highly recommend giving them a copy of our book, Create A Fertile Life. It is evidence-based, easy to read, and you can read from any chapter that is relevant to your circumstances. Purchase your copy and get a head start.
For those of you using clinic-recruited donor sperm, it emphasises the importance of undertaking your own preconception screening and individualised preconception care so that we can optimise egg quality and your endometrial lining to increase the chances of successful implantation.
So, you’ve determined IUI is for you or it has been recommended by your fertility specialist. Did you know that IUI can be performed with or without…
Want to keep reading? Sign up to get instant free access to Sage’s preconception article series and find out about the intricacies of egg freezing, your menstrual cycle, sperm donor considerations, intercourse, conception, egg quality, egg carrying considerations, assisted reproductive technology, home insemination, the answers to your questions and more.
Written by Fertile Ground fertility Naturopath, Sage King.