As a counsellor, listening to and being present to the unfolding stories after a pregnancy ends too early, or when a baby dies, requires me to hold space for another’s sorrow in a way that can seep in, grow, and be held as a deepening sadness. This impact can be felt, yet remain as invisible and silent as the way society responds to these unspeakable losses.
Before you know kindness as the deepest thing inside, you must know sorrow as the other deepest thing.
Naomi Shihab Nye
Supporting someone after a baby dies as a loved one requires holding compassion for any perceived failings in supporting the unravelling of another in sinking downwards into an unfamiliar terrain. Allow them to decide whether to rise again or not and just be there alongside, being the doula for the other side of birth where a baby is missing in every part of their imagined shared futures. It is bleak and dark and unbearable and yet bear it you must as it is only a fraction of what the other carries.
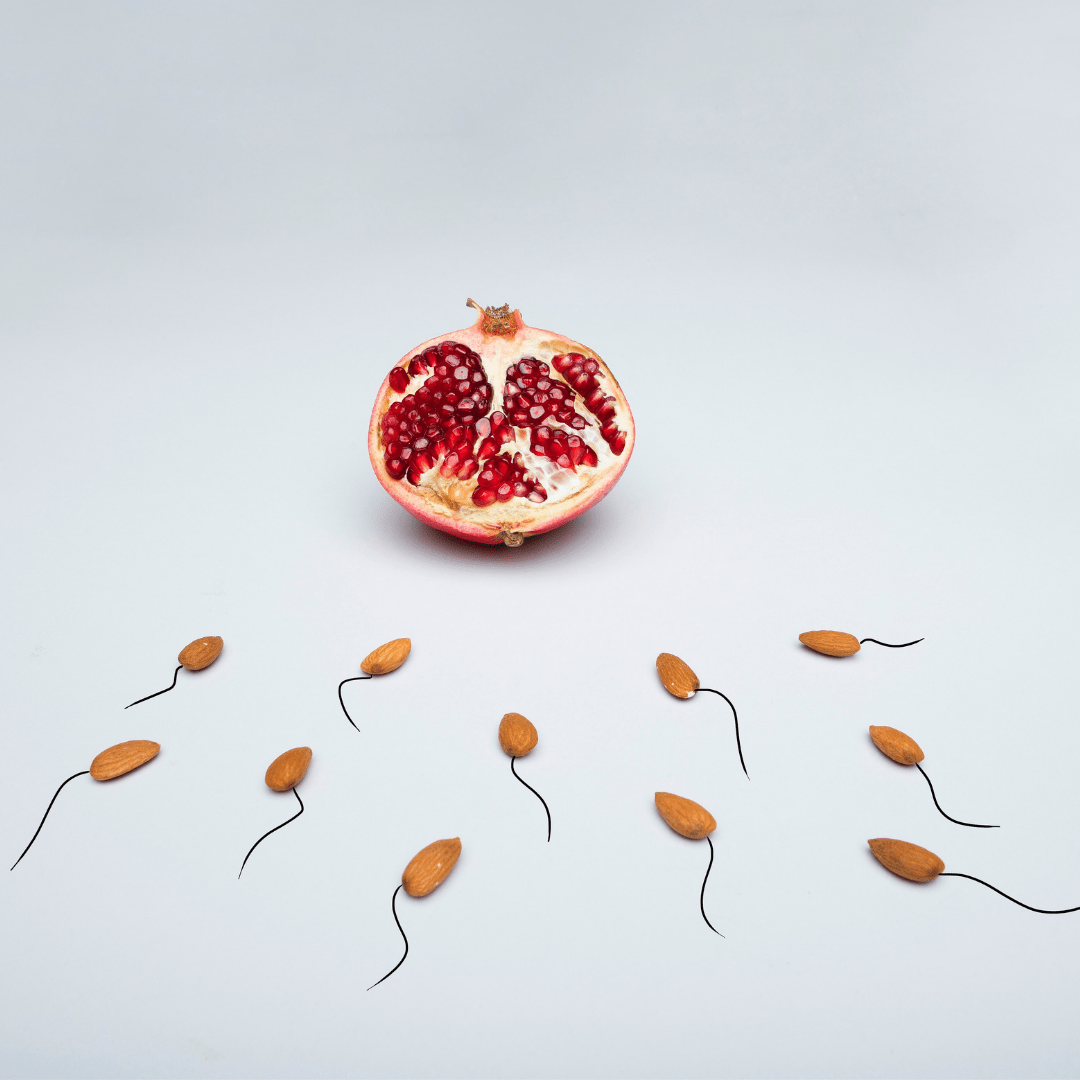
Often the joy of having babies is preceded with experiences of grief, and yet we only see the images around us of blissfully expectant mothers and smiling parents with their children. So rarely do we see the stories of loss, often born shrouded in silence such as with miscarriages, terminations or when a baby dies in utero, during birth or shortly after.
If you visit a maternity hospital, you will likely see image after image of the joy of having a baby. Go seeking a visual representation of the babies that will never be born, die in pregnancy, in labour or shortly after birth and you will notice little to no representation for this reality. With life comes death and the lifetimes in between the two are varied and many, yet we only champion live births and happy parents.
Sitting with
Being alongside such experiences is profound in its sadness, and yet there is honour in being a companion to such grief. Sitting with the love lost and the agony felt in letting go is an enormous task to hold. Forgiveness is needed when you fear you might get it wrong as it comes with the territory where ‘getting it right’ does not really exist. It is as much a fantasy as being a perfect mother. There is only what is.
Be present when others cannot be. Be there because there is a need. Hold self-compassion as you cannot be blamed for any failings as who taught you to hold the unbearable? Who taught you to know what to say, not say and when to do and give instead of speaking? When you cannot ‘fix it’ there is no room for questioning, only sitting with, being with, sharing the uncertainty.
Anchor
Allow the depth of despair to be felt and be held. Give them an anchor to secure themselves to. Let them know their rights in honouring the loss, speaking of their loss, to expect to be heard for as long as they need to speak of their pregnancy, their baby, the child missing from the dinner table. Speak their baby’s name, ask them about their cherished one. Find ways to honour this experience, a tree that blooms at this time of year, a memory box full of all that is known and not yet known about their pregnancy, their baby. Allow for meaning making and disbelief to coexist.
Let them know it gets easier, you get to know the grief, recognise its needs, make room for it, be forever changed by it. Know your limits and encourage professional support so they can become more than the sum of their broken parts. Seek help yourself as you begin to feel that deepening sadness seep in and start to grow. You and I cannot ward this off for we are human, and it is too big to wriggle our way out of it. When attending to another’s grief we must attend to our own breaking hearts.
Know that a parent that has endured suffering on the path to parenthood will be better equipped to know something of their child’s suffering and may pass to them what has been learnt in reaching rock bottom and rising again.
What a gift to give to another to reshape suffering into a way to comfort even if you have never received that yourself. Hold light where there is darkness and know if you only offer kindness, it is enough where there is sorrow.
Perinatal & Fertility Counsellor & Supervisor
Fertile Ground Health Group
If you would like help navigating grief and loss please feel welcome to make a booking with Suzanne.